Why 'organ chips' could transform cancer treatment and drug testing

This story is part of CBC Health's Second Opinion, a weekly analysis of health and medical science news emailed to subscribers on Saturday mornings. If you haven't subscribed yet, you can do that by clicking here.
Cancer treatments don't always work as expected, leaving patients to suffer side effects of chemotherapy without gaining benefits. Now scientists are exploring whether tiny proxy organs made in the lab from a patient’s own cells can do a better job at predicting treatment success.
These proxy organs, also known as organoids, involve growing a patient’s cells into tissue that organizes itself.
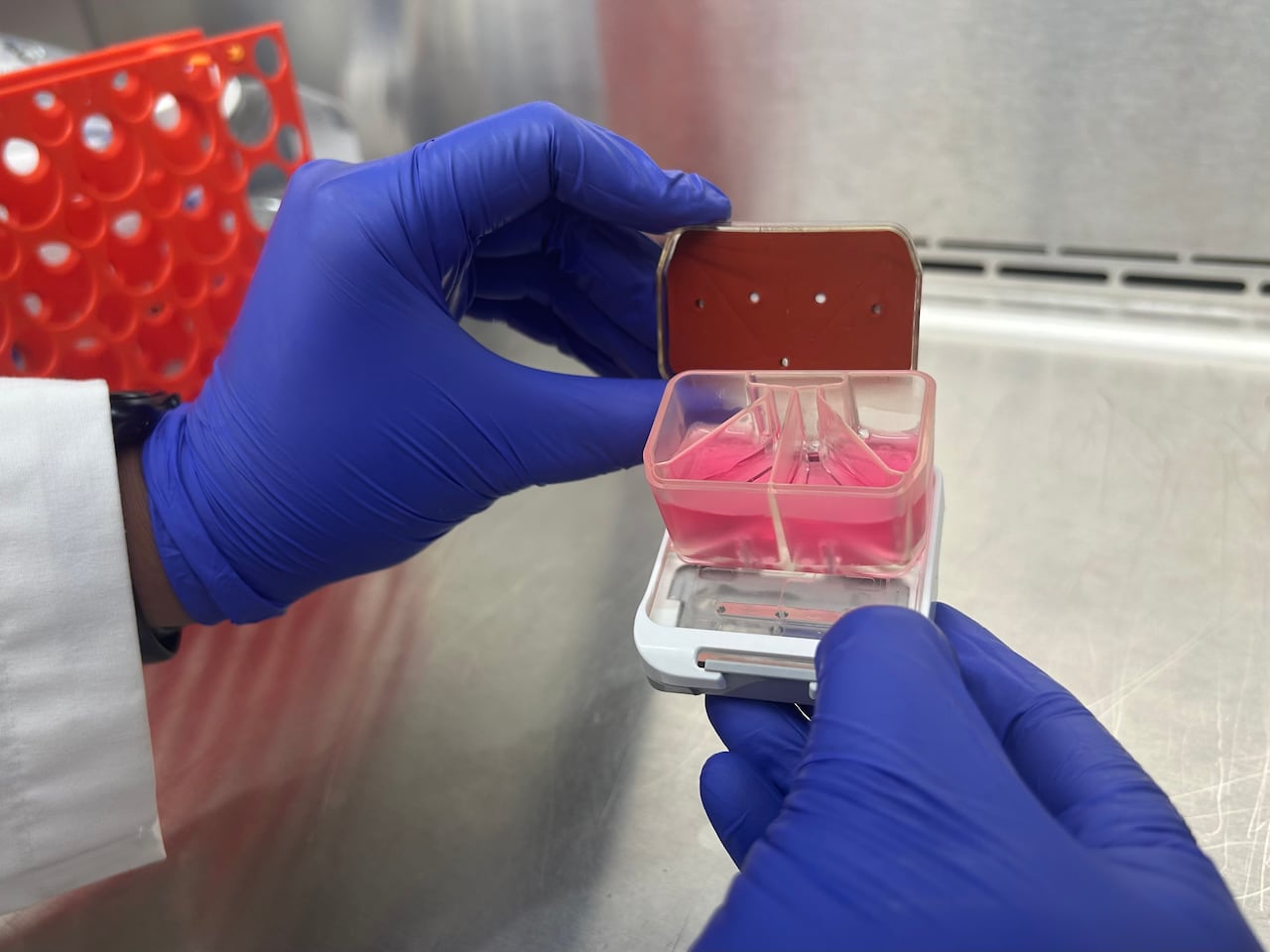
In a more advanced technique, called an organ chip, the organoids are grown on a tiny 3D structure that simulates blood flow. The result? Lung tissue that expands and contract on its own or heart cells beating in unison.
Unlike testing drugs in conventional ways — like human cells growing flat in a dish, or testing on animals — organs on a chip can better capture the complexity of cancer growth and human functions to predict what pharmaceuticals will work safely, medical researchers say.
Here is some of their recent progress amid moves by regulators and politicians in Canada and the U.S. to use fewer animals in experiments.
A team based at Montreal's McGill University and Boston's Harvard University successfully created organoids and a personalized, USB-sized organ chip for eight patients with esophageal adenocarcinoma, a cancer with a high mortality rate.

The experimental tool recreates and grows a patient’s tumour and surrounding tissues with fluid to test how it may respond to treatment.
"We've taken patients' specific tumours, we created their own avatar," said Lorenzo Ferri, director of thoracic and upper gastrointestinal surgery at the McGill University Health Centre. "We showed that we can determine which drugs are effective in that organ chip in four to six weeks and that's the timeline that's important for patients' treatment."
Ferri's team reported recently in the Journal of Translational Medicine that in four chips, the treatment caused death of cancer cells while in the other four, the cells survived.
In the small number of patients they’ve tested so far, those organ chip results lined up perfectly with the patients’ responses to chemotherapy and successful recovery..
Asked how the findings could change his approach to treatment, Ferri said, "I think this is actually transformative."
For now, the experimental technique has only been used in a handful of people. But the idea, Ferri said, to take the guessing out of cancer care.
Allows for personalized treatmentDonald Ingber and colleagues at Harvard's Wyss Institute for Biologically Inspired Engineering developed the patented chip technology for Ferri's experiment.
The chip works by re-creating not just the tumour, but also includes tiny channels for different types of cells plus fluid mimicking blood and connective tissue surrounding. Altogether, it reflects how living cells expand and contract ― important factors that often get missed in traditional lab tests.
Organoids and organ chips could offer a fast-tracked bridge between using lab animals to understand complex organ systems and clinical trial data from humans, said Gordana Vunjak-Novakovic, a university professor of biomedical engineering at Columbia University in New York.
Vunjak-Novakovic and her colleagues used stem cells taken from a blood sample from a child who had cardiomyopathy, a disease of the heart muscle, to create heart tissue on an organ chip with a specific genetic mutation.
"It was a pediatric patient, [a] very young boy," she recalled. After mass screening existing drugs, they found one that should work in his case and /9.6932124shared the information with the boy's cardiologist.
"These are the kind of occasional little successes, but I would expect that actually the whole field will accelerate now when there is so much support from the regulatory side and also from funding side and pharma," Vunjak-Novakovic said.
Shift away from lab animalsIn September, the U.S. National Institutes of Health announced what it called the first dedicated organoid development centre in the U.S. to create standardized and accessible organoid models. The aim is to accelerate drug discovery and add more precise tools for disease modeling, protect public health and reduce reliance on lab animals.
Health Canada and Environment and Climate Change Canada also have a strategy to "replace, reduce or refine ” testing on animals like mice, rats, pigs and dogs.
Ontario Premier Doug Ford has also called for new legislation to ban medical testing on cats and dogs.

Vunjak-Novakovic sees the organoid field progressing to reduce toxicity of drugs for neural diseases and anti-cancer treatments on the heart.
For instance, organoids were used to make safer and better treatments for cystic fibrosis, said Milica Radisic, a professor of biomedical engineering who holds a Canada Research Chair at the University of Toronto.
Radisic and Vunjak-Novakovic hold patents for heart-on-a-chip technology.
By making and maturing tissue, Radisic builds organ chips to mimic diseases of patients from Toronto General Hospital and Hospital for Sick Children, for uses such as in drug testing.
Organoids and organs on a chip allow scientists to figure out what works for a specific patient, Radisic said.
"Tell me about me. That's what people care about, right?" Radisic said.

Currently, the experimental work on the goal of solving a heart disease issue for a family is at the proof-of-concept stage, Radisic said.
In another experiment, Ferri's team at McGill showed that an existing cholesterol-lowering drug can make chemotherapy more effective in some patients.
In the future, cancer research like Ferri's shows the potential to tailor treatments to an individual's genetic makeup, said Kalina Kamenova, a bioethicist who studies public communication of stem cell science.
"In clinical practice, one big issue in the future is going to be how do we scale up this research?" considering cost, said Kamenova, founder and research director of the Canadian Institute for Genomics and Society. "How do we ensure that it brings benefits for everyone in society, for everyone who needs this kind of treatment?"
To start to answer those questions, Ferri's lab already receives courier shipments of tumour samples from patients in Ontario and Manitoba with plans to add British Columbia.
Ferri acknowledged the technology currently costs up to $30,000 per patient sample. Radisic said robots growing organoids could start to take on the tedious daily maintenance of keeping the cells alive under sterile conditions, which could bring costs down.
Opinions vary on if and when organ chips might be able to replace the use of animals in biomedical research.
"The aspect of animal welfare often gets neglected," Radisic said. There's a "real opportunity" in the next 20 to 30 years to really cut back on the number of animals that are used in drug discovery, she said.
cbc.ca





